Endometriosis: Symptoms, treatment, and pain management
What is endometriosis?
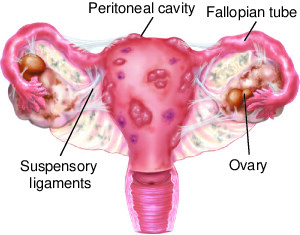
Endometriosis is a painful medical condition that usually affects the lower abdomen or pelvis. But, it tends to affect any body part. It is a condition where the endometrium tissue (lining inside the uterus) abnormally grows outside the uterus. The tissue thickens, breaks down, and bleeds every month with each menstrual cycle. The tissue gets trapped after failing to exit the body. As a result, it causes mild to severe pain, mainly when menstruating.
Endometriosis negatively impacts the functioning and structure of ovaries, fallopian tubes, and other reproductive organs. Typically, the tissue is not cancerous. In case of having surrounding tissues agitated, the scarring and adhesions can spread. The ingrown/swollen/thickened tissue causes blockage in the fallopian tubes leading to abnormal blood build-up, resulting in cysts. The patient might also face infertility issues. The second major complication of endometriosis is Ovarian cancer.
It usually happens when the woman starts menstruating unnecessarily at an early age or having menopause at an older age. The key risk factors are short and heavy menstrual cycles, underweight, higher estrogen levels, and reproductive tract syndromes.
What causes endometriosis?
Till now, science has not been able to diagnose the correct cause of endometriosis, but with hundreds of research, specific possible explanations have been created. Let’s see what the underlying causes of endometriosis are.
- One of the most common theories is “coelomic metaplasia.” It supports the notion that cells outside the uterus usually experience specific modifications or changes, turning them into cells lining the uterus.
- On the top of the list is “retrograde menstruation,” where the menstrual period blood starts flowing back to the pelvic cavity through fallopian tubes rather than being discharged out of the body. As this blood contains endometrial cells, their backflow makes them attach to the pelvic lining. The cells continue to grow and solidify, resulting in thickened uterus tissues.
- Now comes the “induction theory,” featuring a drastic and disturbing transformation of peritoneal cells (cells lining the uterus/pelvic) due to hormonal changes or certain immune factors.
- Apart from abdominal cells, Embryonic cell transformation is known to play a significant role, as well.
- After a hysterectomy, C-section, or any other surgery, the woman can experience attachment of endometrial cells to a surgical incision.
- Immune system disorder: Your immune system fails to identify and terminate endometrial-like tissue that has been growing outside the uterus.
Endometriosis symptoms
Symptoms can either be constant or recurring. The bowel and bladder symptoms are most common. They might improve with time but worsen in menstrual periods. The typical signs and symptoms of endometriosis include:
- Dysmenorrhea OR Painful periods featuring intense pelvic pain and cramping
- Excessive bleeding
- Lower back pain accompanied the abdominal pain.
- Dyspareunia – Discomfort and pain during intercourse or after having sex
- Dyschezia – Painful bowel movements or bouts of pain when urinating, especially in menstrual periods
- Blood in the stool or urine
- Possibly atypical vaginal bleeding
- Spotting or bleeding between periods
Associated symptoms:
- Fatigue
- Diarrhea
- Constipation
- Bloating or nausea
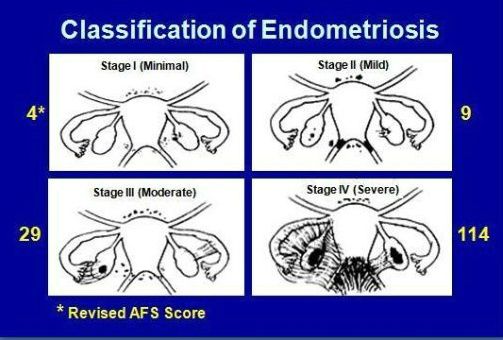
Stages of endometriosis
There are 4 stages of endometriosis.
Stage I – minimal
Secluded implants with few or no significant lesions and adhesions. No evident scar tissues observed.
Stage II – mild
Small but more lesions (Superficial implants) can be seen on the peritoneum and ovaries with no scar tissue and significant adhesions. Typically, almost 2 inches of the abdomen is affected.
Stage II – moderate
Multiple slightly deeper lesions accompanied (in some cases, lesions can be deeply invasive) with endometriomas (cysts) and scar tissue surrounding ovaries and fallopian tubes. Adhesions might become visible.
Stage IV – severe
Multiple lesions (superficial and deep) with large ovarian cysts. The adhesions/scar tissue get dense and filmy.
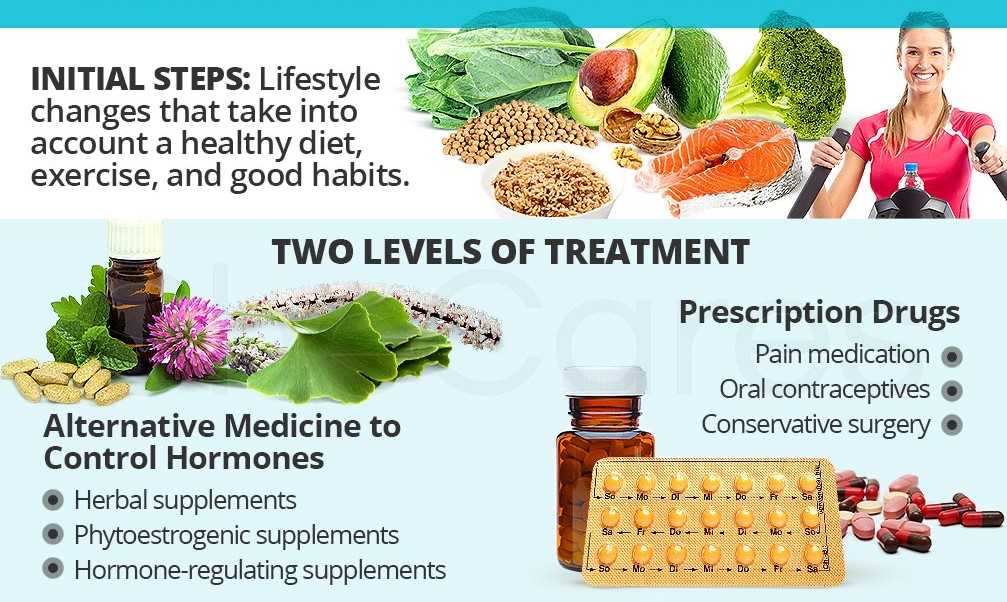
Endometriosis treatment
Medications
Medications have been found extremely valuable in lowering pain. Usually, NSAIDs (nonsteroidal anti-inflammatory drugs) are prescribed, including ibuprofen and naproxen sodium. They help alleviate pain and even associated swelling. For a woman with cysts and infertility, other medications are available.
Hormonal treatment
Apart from NSAIDs, it is treated with hormones that could be birth control pills. If hormonal therapy is considered suitable, the intrauterine device (IUD) tends to release hormones. Depending on the condition, gonadotropin-releasing hormone agonists are also helpful.
Such treatment takes the estrogen levels under control to minimize undesirable tissue development.
Fertility treatment
For infertility, in-vitro fertilization is the best option. And equally safe.
Surgical removal
The very last resort to get rid of endometriosis is removal (excision) done through extensive surgery. It is done to eliminate unwanted tissue growth or scar tissue. With the removal of tissues, the ovaries and fallopian tubes get back to their regular positions, relieving pain.
It is usually the preferred option for women who want to get pregnant. But if you are not planning to have a child, rather than removing tissue, the uterus, ovaries, and fallopian tubes are removed through a procedure called hysterectomy.
Beneficial Dietary approach
- Go gluten and dairy-free
- Maximize intake of fresh fruits and vegetables
- Avoid eating processed or junk food
- Always make a new meal with fresh ingredients
- Limit caffeine intake
- Avoid alcohol consumption
- Try following the regimen of low-FODMAP diet
How do I know if I have endometriosis?
The best indicator is the severity of the pain the patient may experience. Having heavy periods with a gap of fewer than 27 days can be reliable indicators, too. Till now, no specific tests have been formulated to confirm its diagnosis. Proven diagnostic strategies are:
- A comprehensive pelvic examination (structure and function)
- Imaging tests (ultrasound or MRI)
- Surgical laparoscopy (minimally invasive procedure)
- Biopsy
How to cure endometriosis naturally?
Heat: The use of heat through hot baths, hot water bottles, or heat wraps and pads for relaxing the muscles (pelvic and abdominal) and menstrual cramps.
Castor oil: Apply Castor oil directly to the abdomen. Use it at the very initial stage of endometriosis and only before the menstrual flow. It is beneficial in getting rid of extra and abnormal tissue growth.
Turmeric: Being a potent anti-inflammatory food, it alleviates endometriosis symptoms. Ideal to become a part of long-term treatment, the best options for turmeric are turmeric capsules or turmeric tea.
Pick anti-inflammatory foods: Green leafy vegetables, broccoli, celery, blueberries, salmon, ginger, bone broth, chia seeds.
Pelvic massages: Take a few drops of soothing lavender essential oil and massage gently for up to 15 minutes. It helps reduce the tension of pelvic muscles along with reducing inflammation and menstrual cramping.
Ginger tea: Apart from turmeric tea, drink ginger tea two to three times every day. It treats nausea.
Use of herbs and roots: Curcumin, Pine Bark, Chamomile, Peppermint, Vitex, Ashwagandha
Endometriosis Pain Management
For pain relief, there is a wide selection of beneficial approaches. Depending on the severity and associated factors, you can choose the following options for pain management:
- Use an app to track your symptoms
- Maintain a healthy lifestyle with exercise
- Follow a proper regimen of self-care
- Eat your vegetables and fresh fruits
- Understand the science of beneficial fatty acids
- Try acupuncture
- Use a good heating pad for endometriosis

Heat treatment
Using heat is considered highly beneficial for treating pain caused by endometriosis. The sources of heat can vary but applying warmth to the affected area helps in multiple ways. For instance, it relaxes muscles, causes vasodilation, supports healthy blood flow, and reduces pain and stress.
By using heating pads and wraps
It relaxes and soothes the tensed muscles in the pelvic area. It is the safest and most commonly used trick. A heating pack is the best remedy for pain. Moreover, a wireless or electric heating pad should be the priority. If you don’t want to buy one from the market, make your heating pad with rice, flax seeds, or corn. Take a sock and fill it with the desired filler. Heat it in the microwave and use it. Complete solution for aching muscles!
Hot bath
Warm or hot baths are a successful alternative to heating pads. Moist heat has a higher tendency to absorb. It eases pain.
Transcutaneous Electrical Nerve Stimulation (TENS) unit
Are you done with eating pills? Do you feel like giving up on medication? Or are you afraid of drugs? Don’t worry! You can try TENS.
TENS (Transcutaneous electrical nerve stimulation) machines are safe, guaranteed, practical, feasible, recommended, and successful alternatives to painkillers. These small and unobtrusive apparatuses emit vibrations or mild electrical pulses when attached to the skin. These pulses either stop the pain signals from reaching the brain or support the body in producing endorphins-natural pain-fighters. It is not a painful process at all. You might feel ticklish.
- POWERFUL THERAPY
- CUSTOMIZED CONTROL
- TENS TECHNOLOGY
- PORTABLE
- CONVENIENT
- LONG LIFE PADS
Prices pulled from the Amazon Product Advertising API on:
Product prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.
Exercise and Physiotherapy
Following a specified program based on feasible exercise and beneficial relaxation techniques designed by your expert physiotherapist can help control pain and strengthen the pelvic floor and abdominal muscles. Regular exercising based on walking, stretching, and breathing exercises can make you feel better.
The additional benefits are stress management and control of anxiety. Moreover, to lower the pain caused after surgery, gentle exercises, yoga, or Pilates are recommendable.
Additional Questions
Which pain relief medicines are most effective for endometriosis?
Endometriosis pain is typically managed with nonsteroidal anti-inflammatory drugs (NSAIDs). These include over-the-counter options like **ibuprofen, aspirin, and naproxen**. There are also prescription NSAIDs which can be recommended by your healthcare provider depending on the severity of your symptoms. From personal observation, I’ve seen patients respond well to these medications. They help to reduce inflammation and alleviate the discomfort associated with endometriosis. As each person’s body may respond differently to medication, it’s crucial to consult with a healthcare provider before starting any new medication regimen.
What medical approaches are used in dealing with endometriosis pain?
Doctors often suggest **hormone therapy** as an effective way to alleviate endometriosis-associated pain. These hormones can be administered through various methods such as tablets, injections, or even nasal sprays. By inhibiting the production of hormones like estrogen from ovaries, hormone therapy prevents ovulation. This process eases the pain to a great extent. As a medical professional, we have found this route to be effective in numerous cases because endometriosis tissue responds to hormone fluctuations similar to endometrial tissue within the uterus.
Which treatment is considered the first choice for managing endometriosis pain?
The most recommended primary treatments for pain caused by endometriosis include OCPs (Oral Contraceptive Pills), **progesterone-only OCPs, and medroxyprogesterone acetate (Provera)**. As a member of the medical community, I can tell you that these are the standard, first-line treatment options that most healthcare providers turn to when faced with cases of endometriosis. They have proven efficient in controlling and managing the discomfort associated with this condition.
How can chronic pain associated with endometriosis be treated?
Dealing with chronic pain from endometriosis typically involves pain management and **hormone therapy**. Given the fact that endometriosis tissues are influenced by hormones just like the endometrial tissues within the uterus, hormone changes that arise from menstrual cycles can amplify the pain from endometriosis. This is why effective management through hormone therapy and pain mitigation is pivotal. As someone who has worked closely with patients suffering from this condition, I can assure you that these are the most common non-surgical interventions that have shown significant promise in curbing endometriosis pain.

Annika Ramos is a physiotherapist with a passion for helping people recover from injuries and illnesses. In her spare time, she enjoys exploring her creative side through various craft projects.